The soft tissue of the mouth is normally lined with mucosa, which is a special type of skin that should appear smooth in texture and pink in color. Any alteration of the color or texture of the mucosa (lesion) may signal the beginning of a pathologic process. These changes may occur on the face, neck, and areas of the mouth (e.g., gums, tongue, lips, etc.). The most serious of these pathologic changes (which may or may not be painful) is oral cancer. The following can be signs of a suspicious pathologic process such as oral cancer:
Depending on the history, clinical and possibly radiographic exam, your doctor will determine if there are cell changes present, the doctor will take a biopsy of the affected area and send it away to be analyzed by laboratory specialists. When definitive results are obtained, the course of treatment can be determined.
If you are experiencing any pain or symptoms that cause you concern, we encourage you to contact us today to schedule an appointment.
This is the generic term for the set of 3rd molars. These “wisdom teeth” may or may not have to be removed. Factors such as decay, inability to keep them clean or not enough room in the arch for them to erupt normally, can all be reasons for extraction of these teeth.
Dental implants provide a permanent solution for missing teeth, relieving the patient from the hassle associated with partial or complete dentures. They are made of titanium. Implants are placed into the jawbone by the oral & maxillofacial surgeon – a surgical specialist. After a period of healing, the implants are used to support teeth that are custom crafted by your dentist. At completion, the teeth look very natural and greatly enhance the patient’s smile. Strong, stable, and durable, dental implants will last many years with proper care.
What can dental implants correct?
- Missing teeth
- Joint pain or bite problems caused by teeth shifting into vacant spaces
- Cosmetic problems with one’s smile
- Problems with chewing, speech, and digestion
- Misaligned facial tissues
What’s the procedure for getting dental implants?
Getting dental implants requires a number of visits over several months. The surgeon will begin by taking x-rays and impressions, or molds, of the jaw and teeth to gather information about bone tissue, gum tissue, and available spacing for implants. Once the implants are crafted from the molds, the surgeon will numb the patient and surgically place them into the bone. Healing and proper bone integration can take up to six months.
Some implants come with pre-attached posts where others may require a second surgery for placement of the posts that anchor the artificial teeth. Once the posts are in place and the mouth is fully healed, the dentist will mount the artificial teeth. Since adjustment may be necessary, several fitting sessions are often required over the course of one to two months. When tooth alignment is confirmed and healing is complete, the dentist permanently secures the artificial teeth to the implant, providing long-term stability and comfort for the patient.
The surgeon will provide care instructions when the treatment is complete. Good oral hygiene, eating habits, and regular dental visits all aid in the life of your new implants.
The soft tissue of the mouth is normally lined with mucosa, which is a special type of skin that should appear smooth in texture and pink in color. Any alteration of the color or texture of the mucosa (lesion) may signal the beginning of a pathologic process. These changes may occur on the face, neck, and areas of the mouth (e.g., gums, tongue, lips, etc.). The most serious of these pathologic changes (which may or may not be painful) is oral cancer. The following can be signs of a suspicious pathologic process such as oral cancer:
- Red patches or white patches or a combination red/white patch in the mouth
- An ulcer or lesion that has persisted for 2 weeks or longer
- A lump or mass that is growing rapidly
- An area that bleeds easily when touched
- A lump or mass that feels “fixed” or does not move easily
- Difficulty in swallowing or hoarseness
Depending on the history, clinical and possibly radiographic exam, your doctor will determine if there are cell changes present, the doctor will take a biopsy of the affected area and send it away to be analyzed by laboratory specialists. When definitive results are obtained, the course of treatment can be determined.
If you are experiencing any pain or symptoms that cause you concern, we encourage you to contact us today to schedule an appointment.
services appointment
The technique for total rehabilitation of the edentulous, known as the All-on-4 treatment concept, is a surgical and prosthetic medical procedure. The concept was developed, institutionalized and systematically analyzed in the 1990s through studies funded by Nobel Biocare in collaboration with a Portuguese dentist Paulo Maló. It consists of the rehabilitation of the edentulous maxilla and mandible with fixed prosthesis by placing four implants in the anterior maxilla, where bone density is higher. The four implants support a fixed prosthesis with 12 to 14 teeth and it is placed immediately on the day of surgery. All-on-4 is a registered trademark of Nobel Biocare.
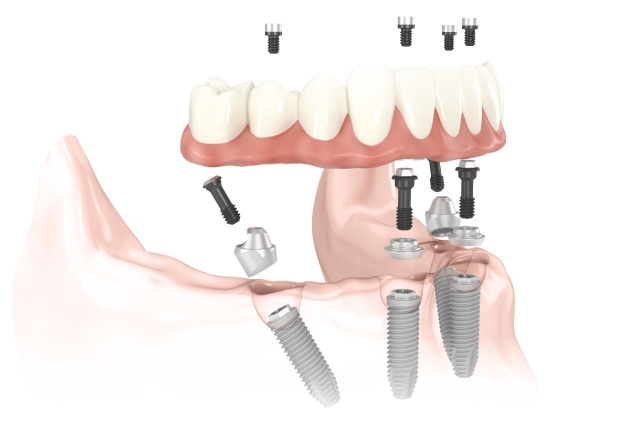
The All-on-4 treatment concept provides a permanent, screw-retained, same-day replacement for the entire upper and / or lower set of teeth. The procedure is best for patients with significant tooth loss or decay and for people whose bone loss in the jaw area prevents them from getting dental implants. Often, tooth loss is accompanied by loss of the jaw bone which poses the problem of reconstruction of the jaw bone. For the implementation to be successful it is necessary to transplant bone from other parts of the body, for example, the iliac crest or the skull and apply it in the area where it is planned to deploy tooth or teeth. Transplantation of bone graft technique takes between three and six months so that the implants can be placed. After implant placement, it is necessary to wait two to three months, after which time it is possible the placement of the fixed prosthesis.
The All-on-4 treatment concept owes its name to the very nature of the method, which consists of applying a dental prosthesis with at least twelve teeth (bridge) fixed in the jaw, based only on four titanium implants.
The specific implants or pillars used by Malo are protected by international patenting.
Obstructive sleep apnea is the most common form of apnea. Here’s information to help you understand how obstructive sleep apnea can affect your life and what can be done about it.
What Is Sleep Apnea?
Apnea literally means “cessation of breath.” If you have sleep apnea, your breath can become very shallow or you may even stop breathing while you are asleep. This state of not breathing can occur up to hundreds of times a night in some people.
What Is Obstructive Sleep Apnea?
Obstructive sleep apnea (OSA) — also called obstructive sleep apnea syndrome — occurs when there are repeated episodes of complete or partial blockage of the upper airway during sleep. During a sleep apnea episode, the diaphragm and chest muscles work harder to open the obstructed airway and pull air into the lungs. Breathing usually resumes with a loud gasp, snort, or body jerk. These episodes can interfere with sound sleep. They can also reduce the flow of oxygen to vital organs and cause irregular heart rhythms.
What Are the Symptoms of Obstructive Sleep Apnea?
Often the person with obstructive sleep apnea is not the first to recognize the signs. OSA is often first noticed by the bed partner or a person who observes the patient at rest. Many people who have OSA have no sleep complaints.
The most common obstructive sleep apnea symptoms include:
- Daytime sleepiness or fatigue
- Dry mouth or sore throat upon awakening
- Headaches in the morning
- Trouble concentrating, forgetfulness, depression, or irritability
- Night sweats
- Restlessness during sleep
- Sexual dysfunction
- Snoring
- Sudden awakenings with a sensation of gasping or choking
- Difficulty getting up in the mornings
Symptoms of OSA in children may not be as obvious. They include:
- Bedwetting
- Choking or drooling
- Excessive sweating at night
- Inward movement of the ribcage when inhaling
- Learning and behavioral disorders
- Poor school performance
- Sluggishness or sleepiness (often misinterpreted as laziness in the classroom)
- Snoring
- Teeth grinding
- Restlessness in bed
- Pauses or absence of breathing
- Unusual sleeping positions, such as sleeping on the hands and knees, or with the neck hyperextended
What are TMJ Treatments?
TMJ Disorder or Temporomandibular Joint Disorder is pain in the area of the lower jaw where the head and jaw connect. The pain experienced may be a result of muscles in the area, problems with the joint or pain in the face around that area. TMJ Disorder can cause severe pain, soreness and problems with speech.
Some of the causes for pain and soreness in the area are:
- Misaligned teeth
- Tension from grinding or clenching
- Stress
- Injury
- Arthritis
Treatments
Although some of the pain in the TMJ area subsides over time, sometimes the pain will remain. Some steps can be taken to help relieve discomfort:
- Use ice packs and mild heat packs
- Eat soft foods
- Relaxation of the jaws – avoid extreme movements or jaw clenching
- Mouthguards/Nightguards
- Pain medication
If mild treatments do not work, other options such as surgery or referral to a physician may be explored. Consult with your dentist if you are experiencing discomfort in the TMJ area.
Wisdom teeth are the third and final set of molars that most people get in their late teens or early twenties. Sometimes these teeth can be a valuable asset to the mouth when healthy and properly aligned, but more often, they are misaligned and require removal.
When wisdom teeth are misaligned, they may position themselves horizontally, be angled toward or away from the second molars, or be angled inward or outward. Poor alignment of wisdom teeth can crowd or damage adjacent teeth, the jawbone, or nerves.
Anatomy of the Teeth
The teeth are the hardest substances in the human body. Besides being essential for chewing, the teeth play an important role in speech. Parts of the teeth include:
- Enamel: The hardest, white outer part of the tooth. Enamel is mostly made of calcium phosphate, a rock-hard mineral.
- Dentin: A layer underlying the enamel. Dentin is made of living cells, which secrete a hard mineral substance.
- Pulp: The softer, living inner structure of teeth. Blood vessels and nerves run through the pulp of the teeth.
Wisdom teeth also can be impacted — they are enclosed within the soft tissue and/or the jawbone or only partially break through or erupt through the gum. Partial eruption of the wisdom teeth allows an opening for bacteria to enter around the tooth and cause an infection, which results in pain, swelling, jaw stiffness, and general illness. Partially erupted teeth are also more prone to tooth decay and gum diseas,e because their hard-to-reach location and awkward positioning makes brushing and flossing difficult.
How Do I Know if I Have Wisdom Teeth?
Ask your dentist about the positioning of your wisdom teeth. He or she may take an X-ray periodically to evaluate for the presence and alignment of your wisdom teeth. Your dentist may also decide to send you to an oral surgeon for further evaluation.
Your dentist or oral surgeon may recommend that your wisdom teeth be extracted even before problems develop. This is done to avoid a more painful or more complicated extraction that might have to be done a few years later. Removal is easier in young people, when the wisdom teeth roots are not yet fully developed and the bone is less dense. In older people, recovery and healing time tend to be longer.
How Are Wisdom Teeth Removed?
The relative ease at which your dentist or oral surgeon can extract your wisdom teeth depends on their position and stage of development. Your oral health care provider will be able to give you an idea of what to expect during your pre-extraction exam. A wisdom tooth that is fully erupted through the gum can be extracted as easily as any other tooth. However, a wisdom tooth that is underneath the gums and embedded in the jawbone will require an incision into the gums and then removal of the portion of bone that lies over the tooth. Often, for a tooth in this situation, the tooth will be extracted in small sections rather than removed in one piece to minimize the amount of bone that needs to be removed to get the tooth out.
What Happens During Wisdom Teeth Removal?
Before your wisdom teeth are pulled, the teeth and the surrounding tissue will be numbed with a local anesthetic — the same type used to numb a tooth prior to having a cavity filled. In addition to the local anesthetic to numb the pain, you and your dentist or oral surgeon may decide that a sedative is desired to control any anxiety. Sedating medications that could be selected include: nitrous oxide (otherwise known as “laughing gas”), an oral sedative (for example, Valium), or an intravenous sedative (administered via an injection into your veins). If nitrous oxide is given, you will be able to drive yourself home. If any of the other medications is selected, you will need someone to drive you both to and from the appointment.
Bone grafting is often closely associated with dental restorations such as dental implants. In the majority of cases, the success of a restoration procedure can hinge on the height, depth, and width of the jawbone at the implant site. When the jawbone has receded or sustained significant damage, the implant(s) cannot be supported on this unstable foundation and bone grafting is usually recommended for the ensuing restoration.
There are several major factors that affect jaw bone volume:
- Periodontal Disease – Gum disease can affect and permanently damage the jaw bone that supports the teeth. Affected areas progressively worsen until the teeth become unstable.
- Tooth Extraction – Studies have shown that patients who have experienced a tooth extraction subsequently lose bone surrounding the extraction site during the following three years. Loss of bone results in what is called a “bone defect”.
- Injuries and Infections – Dental injuries and other physical injuries resulting from a blow to the jaw can cause the bone to recede. Infections can also cause the jaw bone to recede in a similar way.
Oral Examination
Initially, the doctor will thoroughly examine the affected area in order to assess the general condition of the teeth and gums. If periodontal disease is present or the adjacent teeth are in poor condition, these factors will be fully addressed before the bone grafting procedure can begin. The doctor will also recommend panoramic x-rays in order to assess the precise depth and width of the existing bone. On occasion, a CAT scan may be recommended to determine the bone condition.
What Does Bone Grafting Involve?
There are several sources for obtaining bone grafts.
- Autogenous Bone Graft – Harvested from the patient’s own body (usually from the posterior part of the lower jaw or the chin).
- Allograft Bone Graft – Cadaver or synthetic bone is used in this type of graft.
- Xenograft – Cow bone is used in this type of graft.
The healing period after the bone grafting procedure can take anywhere from 4-6 months to complete. Bone is typically harvested from your own body (or on rare occasions obtained from a “bone bank”) and added to the affected site. This bone will fuse with the existing bone and the migration of cells will cause firm adhesion and cell growth. Supplementing the jaw with bone will result in greater bone mass to help support and anchor the implant(s).
The most common causes of facial injuries include falls, motor vehicle accidents and sports injuries. Injuries to the facial region can impart not only physical injury but emotional trauma as well. Oral and Maxillofacial Surgeons have received a minimum of 4 years of intensive hospital based surgical training and are uniquely trained in repairing both soft tissues (facial lacerations) and bony injuries to maxillofacial region( nose, cheek bones, jaw bones and eye sockets) and oral cavity (intraoral lacerations and knocked out or displaced teeth) to restore function and achieve esthetics.
If facial bones have been fractured or broken, they will be treated in much the same way as any other broken bone. Unlike other bones of the body, a plaster cast cannot be applied to a cheekbone, but the bones can be held firmly together by either wiring or the insertion of small plates and screws. Soft tissue lacerations are treated immediately by way of suture (stitching). Depending on the nature of the injury, treatment can take place in the hospital or in the office.
Does the thought of having your teeth cleaned make your entire body tense with fear? Would you rather endure the agony of a toothache than step foot in a dentist’s office? You’re not alone. A lot of people are so phobic about going to the dentist that they prefer not to have any treatment.
For people who avoid dentists like the plague, sedation dentistry may take away some of their anxiety. Sedation can be used for everything from invasive procedures to a simple tooth cleaning. How it’s used depends on the severity of the fear.
What Is Sedation Dentistry?
Sedation dentistry uses medication to help patients relax during dental procedures. It’s sometimes referred to as “sleep dentistry,” although that’s not entirely accurate. Patients are usually awake with the exception of those who are under general anesthesia.
The levels of sedation used include:
- Minimal sedation — you are awake but relaxed.
- Moderate sedation (formerly called “conscious sedation”) — You may slur your words when speaking and not remember much of the procedure.
- Deep sedation — you are on the edge of consciousness but can still be awakened.
- General anesthesia — you are completely unconscious.